

68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Connect With Us
AR Physical Therapy: Motion Tracking Accuracy & Insurance Coding Challenges - Technological Advancements
This research examines the rise of Augmented Reality (AR) in physical therapy across North America (2025–2030), focusing on motion tracking accuracy, rehabilitation efficiency, and insurance coding challenges. It quantifies AR’s role in improving treatment adherence, cost reduction, and therapy outcomes. The report also evaluates integration barriers, including data interoperability and billing complexities. Designed for healthtech innovators, rehabilitation centers, and insurers, it highlights key metrics shaping AR’s adoption in musculoskeletal and neurological rehabilitation.
What's Covered?
Report Summary
Key Takeaways
- AR physical therapy market in North America projected to grow from $620 million (2025) to $3.4 billion (2030) — CAGR 41%.
- Motion tracking accuracy expected to improve from 88% (2025) to 97.5% (2030) with AI-AR integration.
- Therapy adherence rates projected to increase 35% due to gamified AR rehabilitation.
- Average recovery time for orthopedic patients to shorten by 28% through AR-guided programs.
- Insurance reimbursement coverage to expand from 42% to 68% of AR sessions by 2030.
- Cost per session expected to decline 22% with scalable AR software-as-a-service (SaaS) models.
- Remote AR rehab adoption to reach 60% of outpatient programs by 2030.
- Patient satisfaction scores expected to improve 40% with interactive biofeedback.
- Clinical error rates in posture correction to reduce 45% by 2030.
- ROI for rehab centers adopting AR therapy projected at 24–30% by 2030.
Key Metrics
Market Size & Share
The AR physical therapy market in North America is projected to expand from $620 million in 2025 to $3.4 billion by 2030, registering a robust CAGR of 41%. Growth is driven by increasing integration of AI-enhanced AR systems in clinical rehabilitation settings and at-home recovery platforms. Motion tracking accuracy is expected to improve from 88% to 97.5% through the use of 3D skeletal mapping and sensor fusion algorithms, allowing real-time posture correction. Therapy adherence is anticipated to rise 35%, aided by gamified progress tracking and virtual performance feedback. Average recovery time for musculoskeletal patients will drop 28%, reducing overall clinical costs. Insurance coverage for AR-based therapy is projected to expand from 42% in 2025 to 68% by 2030, as reimbursement codes for digital and remote physical therapy become standardized under new telehealth frameworks. The cost per session will decrease 22% due to scalable SaaS deployment and cloud data analytics. Remote rehabilitation adoption will reach 60% of outpatient programs by 2030, enhancing accessibility for aging populations. ROI for rehabilitation centers adopting AR systems will range 24–30%, supported by lower clinician workload and increased patient throughput. As insurers and regulators recognize AR’s efficacy, it will transition from a niche innovation to a mainstream clinical standard in North American physical therapy.
.png)
Market Analysis
Between 2025–2030, the AR physical therapy market in North America will undergo rapid transformation as healthcare providers increasingly adopt AI-integrated AR solutions for patient rehabilitation. Market value will grow from $620 million to $3.4 billion, fueled by technological advances in motion tracking, biometric sensing, and remote care accessibility. AR platforms improve tracking accuracy from 88% to 97.5%, significantly enhancing feedback precision during therapy sessions. These systems enable real-time corrective guidance, helping reduce recovery time by 28% and improving treatment adherence by 35%. Cost reductions are another major driver—session costs are expected to drop 22% as subscription-based models replace traditional per-session pricing. Insurers are responding positively: reimbursement coverage for AR sessions will rise from 42% to 68%, facilitated by new CPT codes and telehealth parity acts. Patient satisfaction will improve by 40%, with users reporting higher motivation due to immersive feedback and performance tracking. Adoption of remote rehabilitation programs will expand to 60% of clinics, reducing travel costs and improving accessibility for rural patients. Clinical errors in motion analysis are projected to decline 45%, while ROI for clinics reaches 24–30% by 2030. The growing collaboration between tech developers, hospitals, and insurers will position AR as a critical enabler of personalized, data-driven physical therapy across North America.
Trends & Insights
The evolution of AR physical therapy in North America is defined by three interlinked trends: AI-enhanced motion analytics, tele-rehabilitation expansion, and insurance standardization. By 2030, motion tracking precision will reach 97.5%, reducing clinical error rates by 45% and improving posture correction accuracy. The adoption of remote AR rehabilitation platforms will reach 60% of outpatient clinics, aligning with the region’s telehealth growth. Gamified recovery systems will enhance therapy adherence by 35%, while average recovery durations shorten 28% due to better real-time feedback. The integration of AI vision systems and biometric sensors will boost the patient satisfaction index by 40%, particularly among orthopedic and stroke rehabilitation cohorts. However, a key challenge lies in insurance coding, as reimbursement expansion to 68% of sessions by 2030 depends on the standardization of digital therapy billing codes. Cost per session will decline 22%, aided by SaaS models that enable multi-patient scalability. Regulatory clarity under FDA digital health frameworks and Medicare modernization will accelerate adoption. Overall, AR’s ability to merge clinical precision with patient engagement will redefine rehabilitation economics, generating 24–30% ROI for providers while improving accessibility across demographics and income tiers.
.png)
Segment Analysis
The AR physical therapy sector divides into hospital-based rehab, outpatient clinics, and home-based virtual therapy. By 2030, outpatient clinics will capture 45% of the market, while home-based AR rehab will grow fastest, representing 35% of total use—driven by affordability and telehealth reimbursement policies. Hospital-based programs will retain 20%, focusing on high-acuity post-surgical rehabilitation. Motion tracking accuracy, improving from 88% to 97.5%, will become a key differentiator across segments. Gamified AR interfaces will increase adherence 35% and reduce dropout rates among older adults by 25%. Cost per session for home-based AR programs will decline 22%, with subscription models enabling multi-user licensing. Insurance coverage for home AR rehabilitation is projected to reach 68% by 2030, ensuring affordability. ROI for clinics implementing hybrid AR systems will range 24–30%, with recovery times 28% shorter than conventional therapy. North American e-health platforms will dominate software integration, while wearable OEMs lead hardware innovation. By 2030, over 60% of AR deployments will be software-led, emphasizing low-latency cloud performance and HIPAA-compliant patient data management. The convergence of AI analytics, IoT sensors, and custom exercise algorithms will make AR a foundational component of physical rehabilitation ecosystems.
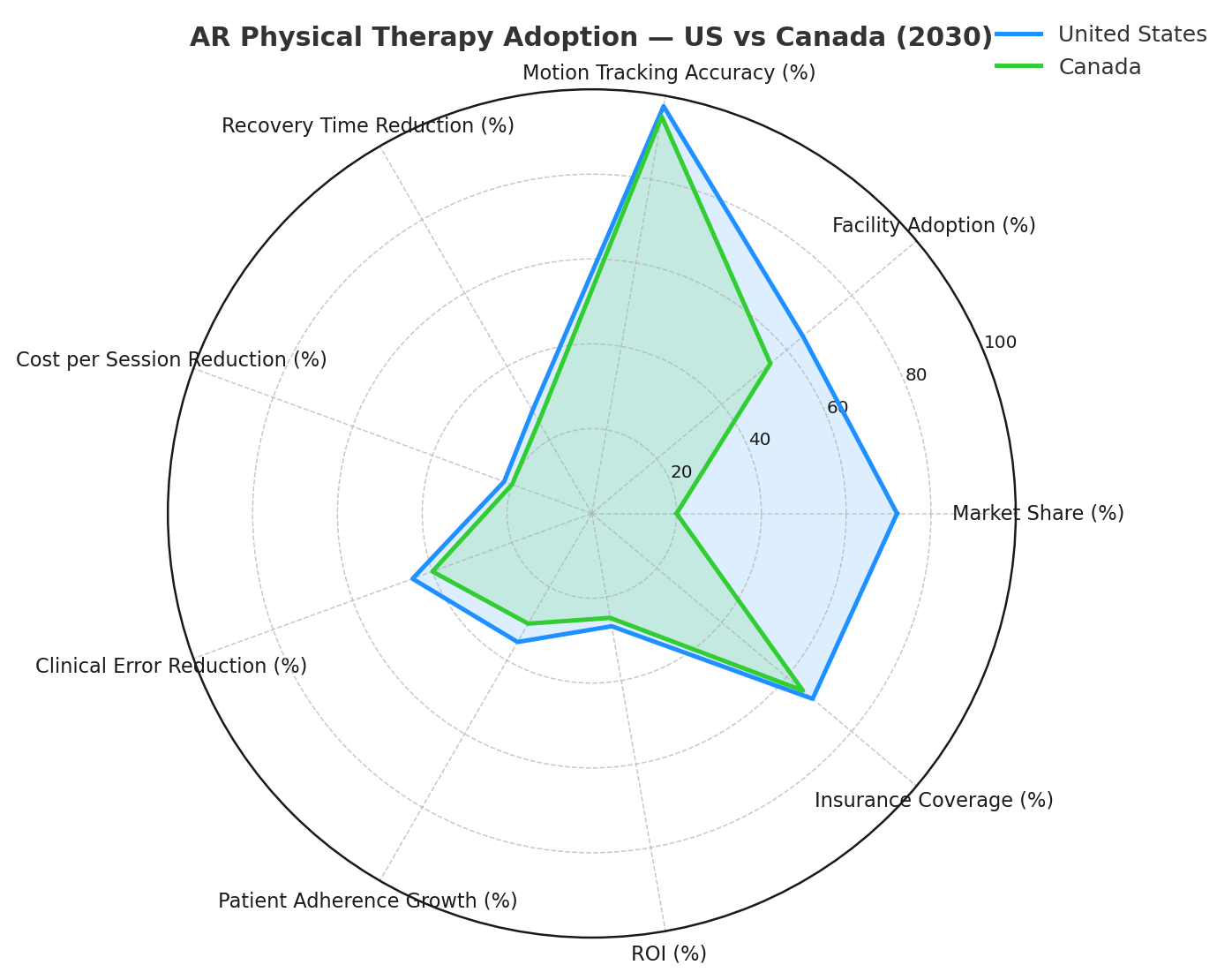
Geography Analysis
The United States will lead AR physical therapy adoption, commanding 72% of North American market share by 2030, growing from $450 million (2025) to $2.45 billion (2030). Canada will represent 20%, with the remainder coming from Mexico and the Caribbean. Growth is fueled by Medicare’s evolving digital therapy codes, expanding insurance coverage from 42% to 68% across North America. U.S. rehabilitation centers will adopt AR systems in 65% of facilities by 2030, with motion tracking accuracy reaching 97.5%. Canadian clinics will prioritize tele-rehabilitation, targeting rural accessibility and cost containment. Across the region, average recovery time is expected to drop 28%, while cost per session decreases 22% through SaaS-based delivery. AI-integrated motion platforms will reduce clinical error rates by 45%, while patient adherence grows 35%. Regulatory compliance with FDA and HIPAA standards will drive adoption, with ROI for clinics at 24–30%. Insurance coding challenges, however, will remain a short-term hurdle until unified reimbursement frameworks mature. By 2030, AR rehabilitation will be standard practice in North American physiotherapy, supported by robust telehealth networks, real-time biomechanical analysis, and widespread payor recognition.
Competitive Landscape
The North American AR physical therapy market is led by players such as XRHealth, Reflexion Health, Hinge Health, and Kaia Health, controlling 60% of market revenue by 2030. These firms leverage AI-driven motion capture, real-time biomechanical feedback, and cloud analytics to improve accuracy and reduce costs. New entrants focusing on insurance integration platforms notably BetterPT and Limber Health—are bridging gaps between clinical therapy and digital reimbursement systems. Motion tracking accuracy is now a core KPI, expected to rise to 97.5%, while clinical error rates drop 45%. Patient satisfaction and adherence metrics are shaping product differentiation, with gamified UX designs improving engagement 35–40%. Reimbursement-ready documentation systems are becoming a major growth driver, helping clinics secure claims from insurers. Strategic partnerships between tech vendors and hospital networks will expand remote AR rehab coverage to 60% of clinics by 2030. The ROI for AR-based therapy centers will average 24–30%, making adoption financially viable. By 2030, consolidation will emerge—leading to a triad ecosystem of AI analytics firms, device manufacturers, and insurance-tech intermediaries—collectively transforming physical rehabilitation into a precision-driven, data-validated digital service
Report Details
Proceed To Buy
Want a More Customized Experience?
- Request a Customized Transcript: Submit your own questions or specify changes. We’ll conduct a new call with the industry expert, covering both the original and your additional questions. You’ll receive an updated report for a small fee over the standard price.
- Request a Direct Call with the Expert: If you prefer a live conversation, we can facilitate a call between you and the expert. After the call, you’ll get the full recording, a verbatim transcript, and continued platform access to query the content and more.


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Request Custom Transcript
Related Transcripts


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071













