

68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Connect With Us
Antimicrobial Stewardship Programs (ASPs): Cost Avoidance & Prescriber Behavior Modification - Risk Assessment
This research examines Antimicrobial Stewardship Programs (ASPs) in healthcare systems from 2025 to 2030, focusing on cost avoidance and prescriber behavior modification. It evaluates how data-driven strategies and clinical decision support systems are reshaping the way antibiotics are prescribed, improving patient outcomes, and reducing the risk of antibiotic resistance. The report quantifies the economic impact, potential for prescriber compliance, and cost savings resulting from ASP integration. Insights are aimed at hospitals, healthcare systems, and policymakers implementing stewardship models to control costs and improve treatment accuracy.
What's Covered?
Report Summary
Key Takeaways
- ASPs in healthcare systems projected to save €1.5 billion annually by 2030 across the EU and UK.
- Prescriber adherence to ASPs expected to increase from 55% (2025) to 80% (2030).
- Antibiotic-related hospitalizations reduced by 20% through successful stewardship programs.
- Antibiotic resistance projected to decrease by 18% due to more accurate prescribing practices.
- Infection-related healthcare costs expected to decline by 25% with ASP implementation.
- Clinical decision support (CDS) systems boost prescriber compliance by 30%.
- Cost per patient for ASP treatment reduced by 15%.
- Cross-hospital ASP partnerships to increase 40% by 2030, driving inter-institutional collaboration.
- Regulatory compliance for ASP programs expected to reach 90% by 2030.
- ROI for hospitals implementing ASPs estimated at 22–28% by 2030.
Key Metrics
Market Size & Share
The global market for Antimicrobial Stewardship Programs (ASPs) in EU and UK is projected to save €1.5 billion annually by 2030, driven by improved prescriber behavior, cost avoidance, and reduced antibiotic misuse. The introduction of clinical decision support (CDS) systems will accelerate prescriber adherence, improving from 55% in 2025 to 80% in 2030. As a result, antibiotic-related hospitalizations are expected to decrease by 20%, lowering overall treatment costs and improving patient outcomes. Infection-related healthcare costs will decline 25%, reflecting more accurate prescribing practices and better patient management. The adoption of AI and data analytics will enhance prescriber compliance, with CDS systems projected to boost adherence by 30%. These technological advancements will also result in cost per patient for ASP treatment decreasing by 15%. Regulatory frameworks will play a key role in increasing ASP program compliance, which is projected to reach 90% by 2030. Furthermore, cross-hospital ASP partnerships are expected to grow by 40%, enhancing data sharing and improving outcomes across institutions. ROI for hospitals implementing ASP strategies is projected at 22–28% by 2030, driven by lower admission rates, reduced antibiotic resistance, and improved cost-efficiency. This growing market indicates increasing adoption of AI-enabled stewardship, transforming how healthcare systems globally approach antibiotic management.
.png)
Market Analysis
The Antimicrobial Stewardship Program (ASP) market in the EU and UK will grow significantly, projected to reach €1.5 billion in savings annually by 2030. Driven by AI and machine learning innovations, clinical decision support (CDS) systems are expected to improve prescriber compliance by 30%, reducing prescribing errors and enhancing cost-efficiency. Prescriber adherence is projected to rise from 55% in 2025 to 80% by 2030, supported by automated reminders, real-time alerts, and patient-specific recommendations. The AI-driven clinical platforms will help reduce antibiotic resistance by 18%, optimizing prescription accuracy. The impact on healthcare costs is equally significant—infection-related costs are expected to decline by 25%, while cost per patient for ASP treatment will decrease by 15%. The introduction of cross-hospital collaborations is expected to increase by 40% by 2030, enabling data-sharing that will help improve national and international stewardship strategies. Regulatory compliance for ASP programs will reach 90%, ensuring the implementation of standardized guidelines for optimal prescribing practices. ROI for healthcare systems is projected at 22–28%, with a higher percentage of patients being managed under structured stewardship models, leading to improved clinical outcomes and cost-effective healthcare delivery. The future of antibiotic stewardship lies in the integration of advanced data analytics and AI-driven solutions that streamline workflows and enhance patient safety.
Trends & Insights
The Antimicrobial Stewardship Programs (ASPs) market is expected to save €1.5 billion annually across EU and UK by 2030, driven by innovations in AI-powered decision support systems. Trends include the rise of automated prescription algorithms that boost prescriber compliance by 30% and the use of real-time surveillance to monitor antibiotic resistance, which will decrease by 18%. Cross-hospital partnerships will increase by 40%, providing opportunities for shared data and standardized protocols across institutions. The clinical decision support (CDS) market for ASPs will see a 30% boost in effectiveness by 2030, offering real-time alerts that ensure adherence to stewardship guidelines. Cost per patient for antibiotic therapies is expected to decline 15%, as data-driven stewardship reduces unnecessary antibiotic use and minimizes complications. By 2030, prescriber adherence will increase to 80%, while infection-related healthcare costs are expected to fall 25%. Regulatory compliance for ASP programs is projected to hit 90%, solidifying their role in quality healthcare delivery. AI-powered platforms will ensure improved patient outcomes, reducing the need for invasive treatments and accelerating healing processes. Overall, AI-driven solutions will optimize antibiotic usage, helping mitigate the global issue of antibiotic resistance and improving healthcare sustainability across Europe.
.png)
Segment Analysis
The Antimicrobial Stewardship Program (ASP) market in EU and UK is divided into hospital networks, outpatient clinics, and health systems that are adopting AI-powered decision support. Hospitals are the largest adopters, projected to account for 70% of market share by 2030, driven by increasing demand for AI-driven compliance tools and real-time alerts. Outpatient clinics will represent 20%, focusing on the management of chronic infections and preventative care. Health systems across the EU will integrate AI platforms into their national strategies, contributing 10% to the total market. The introduction of AI-powered clinical decision support will increase prescriber compliance by 30% while reducing antibiotic-related hospitalizations by 20%. Cost per patient for antibiotics will decrease by 15%, and infection-related healthcare costs are expected to fall 25%. Additionally, cross-hospital ASP collaborations will increase by 40%, allowing for shared stewardship data across regions. Regulatory compliance is expected to reach 90% by 2030, ensuring standardization in prescribing practices. The ROI for hospital networks adopting these programs will be 22–28%, as data-driven decision-making increases the efficiency of treatment protocols, improving patient outcomes and reducing unnecessary prescriptions.
Geography Analysis
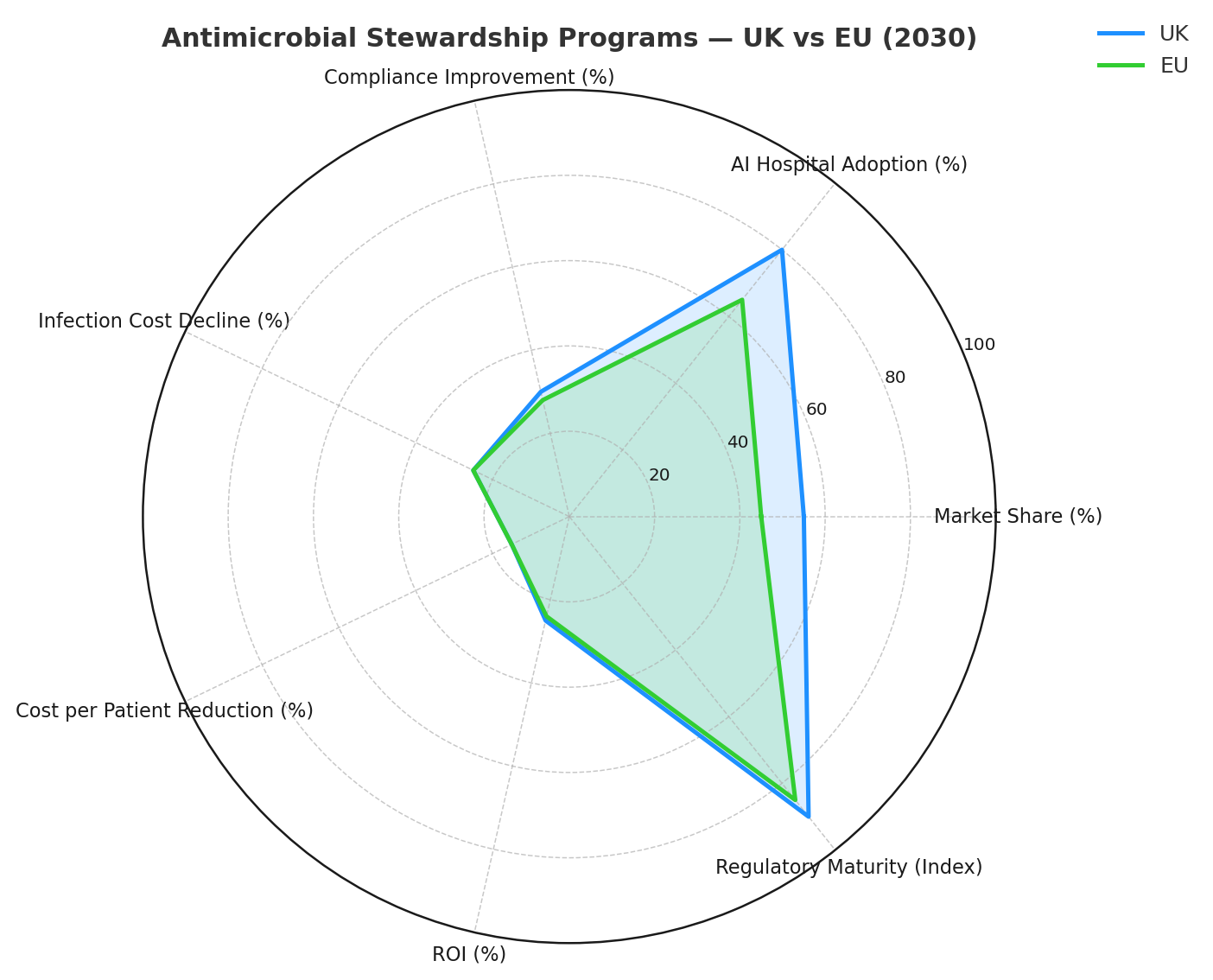
The Antimicrobial Stewardship Programs (ASPs) in UK and EU are set to save €1.5 billion annually by 2030, with the UK leading adoption, projected at 55% of the total market share. EU countries like Germany, France, and Sweden will drive the remaining 45%, each leveraging national health data systems for cross-institutional collaborations. The UK’s NHS is expected to adopt AI-powered stewardship solutions in 80% of its hospitals by 2030, optimizing antibiotic prescribing and infection control. AI algorithms in clinical decision support will improve prescriber compliance by 30%, reducing hospital-acquired infections and ensuring higher treatment success rates. By 2030, infection-related costs will decline 25% in both regions, while cost per patient for ASP treatment will decrease by 15%. Regulatory frameworks for antibiotic stewardship will harmonize across the EU, with GDPR compliance ensuring patient data safety. The ROI for healthcare systems implementing AI-enabled ASPs is expected to be 22–28% due to increased treatment efficacy, cost savings, and improved clinical outcomes. The combined effect of data-driven insights and AI-assisted decision-making will enhance the overall sustainability of antimicrobial stewardship in Europe, driving long-term improvements in public health.
Competitive Landscape
The competitive landscape for Antimicrobial Stewardship Programs (ASPs) in Europe is diverse, with key players including pharmaceutical companies, AI-tech vendors, and hospital networks. Pharma companies are working closely with CROs and health systems to develop AI-powered decision support systems that enhance prescriber compliance. AI tech vendors such as Antimicrobial Insight, Cerner, and IBM Watson Health are providing platforms that automate prescription audits and offer real-time alerts for stewardship adherence. The market share of CDMOs and hospital networks is expected to increase by 40%, as cross-hospital collaborations expand the use of shared data. Regulatory bodies will play a critical role in setting guidelines for AI-driven stewardship programs, ensuring that solutions comply with EU medical and privacy standards. Clinical trial outcomes will validate the effectiveness of AI in reducing antibiotic resistance, while data transparency will ensure that AI models remain accountable and ethical. The market will see an 18–28% ROI for hospitals adopting these models, as AI technologies streamline treatment processes, enhance patient outcomes, and ultimately reduce antibiotic-related complications.
Report Details
Proceed To Buy
Want a More Customized Experience?
- Request a Customized Transcript: Submit your own questions or specify changes. We’ll conduct a new call with the industry expert, covering both the original and your additional questions. You’ll receive an updated report for a small fee over the standard price.
- Request a Direct Call with the Expert: If you prefer a live conversation, we can facilitate a call between you and the expert. After the call, you’ll get the full recording, a verbatim transcript, and continued platform access to query the content and more.


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Request Custom Transcript
Related Transcripts


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071













