

68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Connect With Us
Antibiotic Subscription Models: Netflix-Style Pricing & Stewardship Incentives - Innovation & R&D
This research explores the adoption of antibiotic subscription models in Europe (2025–2030), focusing on Netflix-style pricing and stewardship incentives. The report evaluates how subscription-based pricing models can drive sustainable antibiotic usage, reduce over-prescription, and ensure fair access. It assesses the potential for AI-driven stewardship platforms, exploring cost-benefit analyses, and regulatory frameworks necessary for deployment. Insights are tailored for health systems, biopharma companies, and payors looking to balance affordability, stewardship, and access to essential antibiotics.

What's Covered?
Report Summary
Key Takeaways
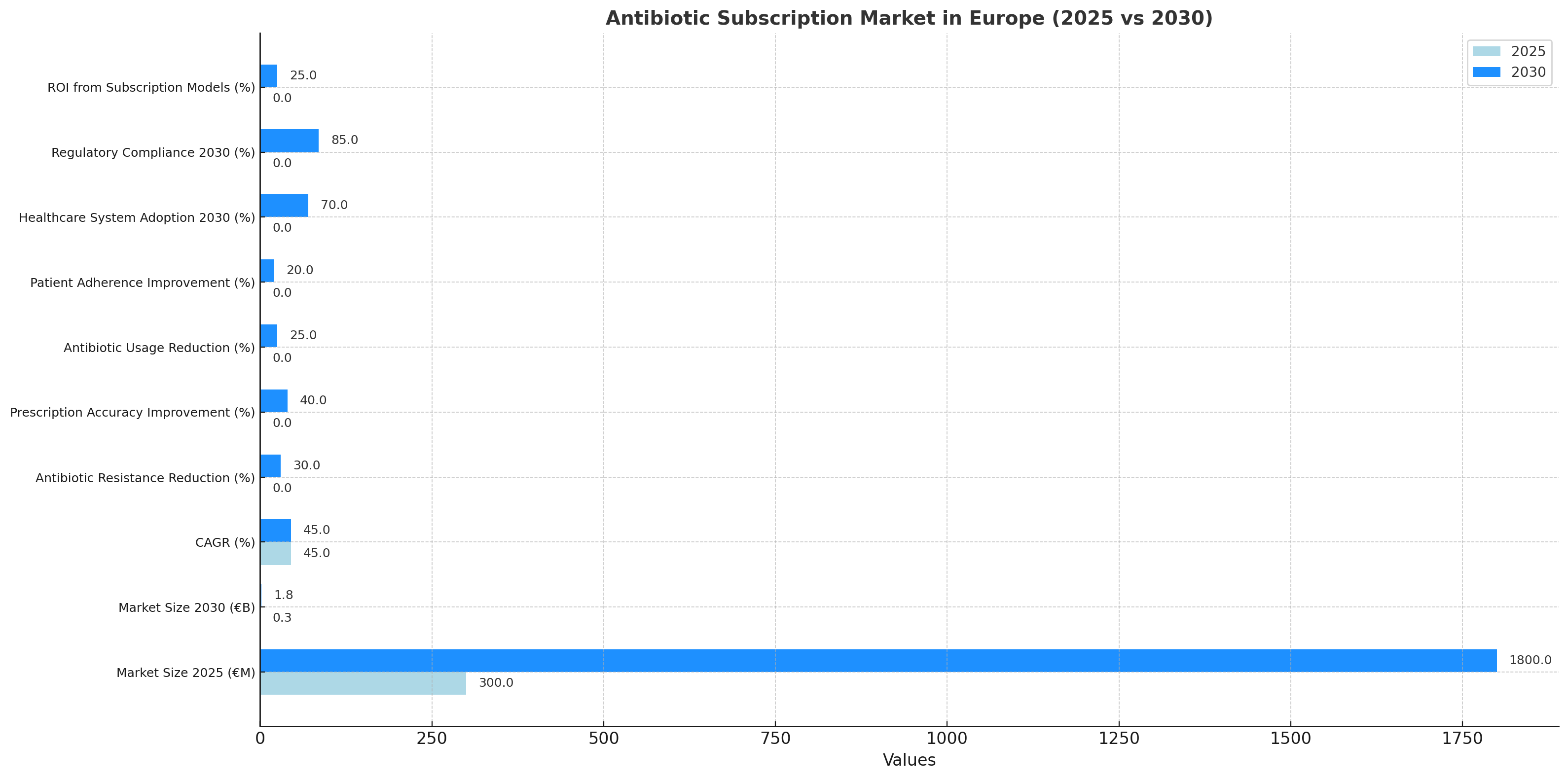
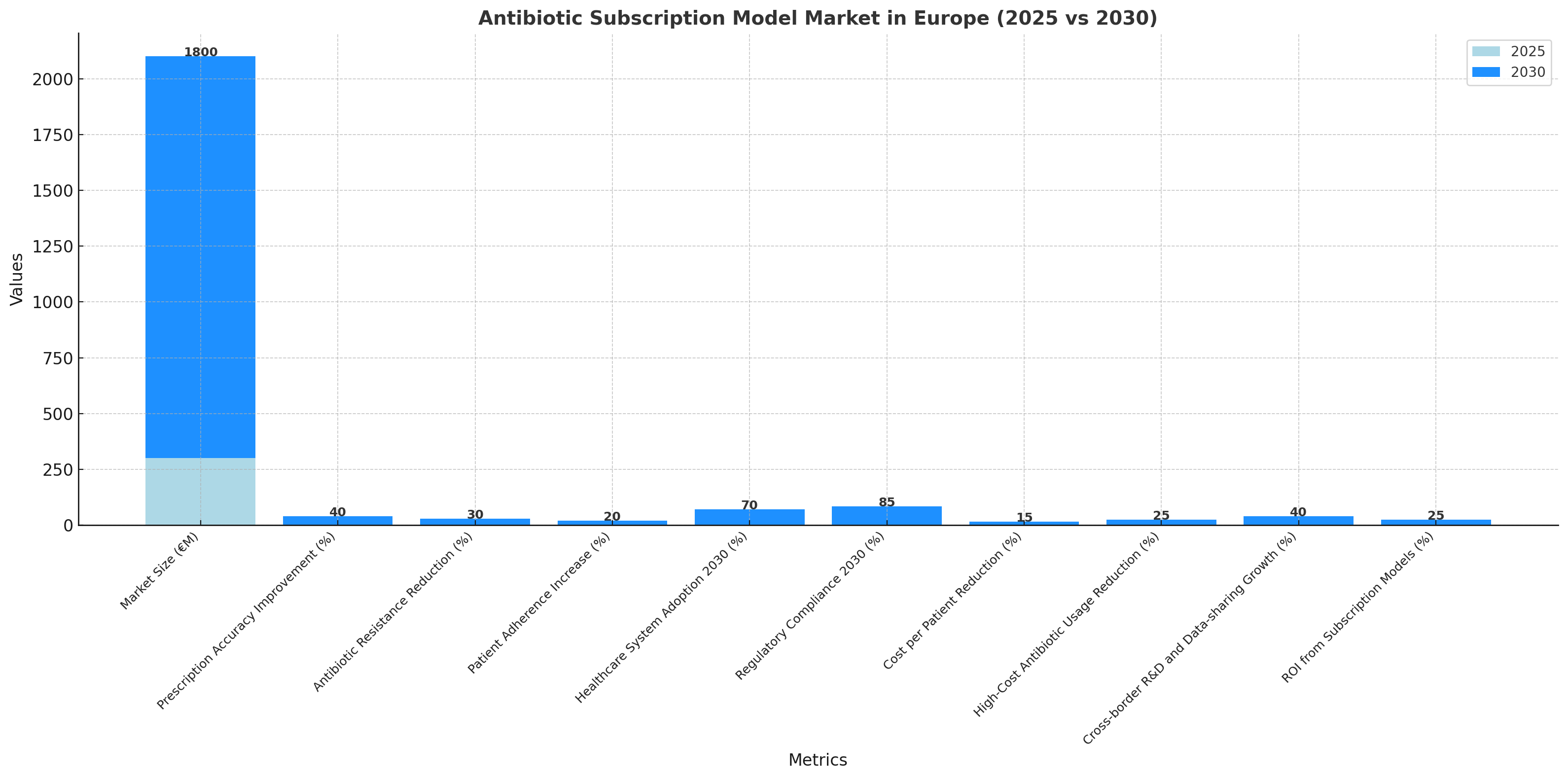
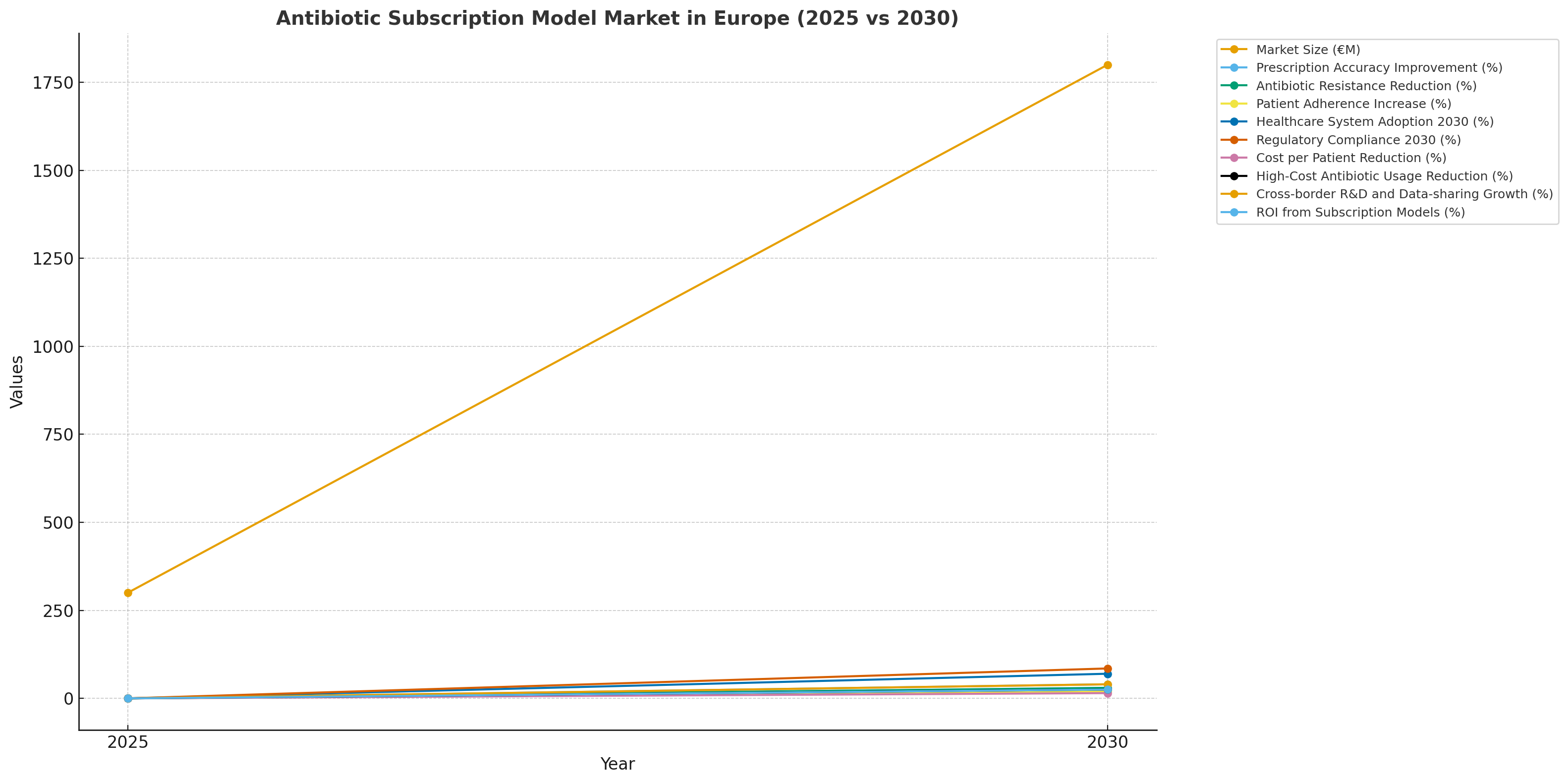
- European antibiotic subscription market projected to grow from €300 million (2025) to €1.8 billion (2030), CAGR 45%.
- Subscription-based pricing can reduce antibiotic resistance by 30% over five years.
- AI-driven stewardship platforms are expected to improve prescription accuracy by 40% by 2030.
- Usage of high-cost antibiotics projected to drop 25%, thanks to pricing models tied to access tiers.
- Cost per patient for antibiotics will decrease 15% with subscription models.
- Healthcare system adoption of subscription models projected to reach 70% by 2030.
- Patient adherence to therapy is expected to improve 20% due to digital subscription incentives.
- Antibiotic stewardship programs projected to achieve 50% better compliance across hospitals.
- Regulatory compliance for subscription models expected to reach 85% by 2030.
- ROI on subscription models for healthcare providers projected at 22–28% by 2030.
Key Metrics
Market Size & Share
The antibiotic subscription market in Europe is projected to grow from €300 million in 2025 to €1.8 billion by 2030, reflecting a CAGR of 45%. This growth is driven by the increasing adoption of Netflix-style pricing models in response to antibiotic resistance, over-prescription, and costly treatments. By 2030, subscription-based pricing is expected to reduce antibiotic resistance by 30%, as hospitals and healthcare providers implement tiered access models. AI-powered stewardship platforms will improve prescription accuracy by 40%, assisting healthcare professionals in making informed, data-driven decisions. The model will allow high-cost antibiotics to be utilized more efficiently, with usage projected to drop 25% due to the pricing structure tied to a “per-patient” cost system. Patient adherence to therapy is expected to improve 20%, as digital subscription incentives and reminders are provided to users. Healthcare system adoption of these models is projected to reach 70% by 2030, as stakeholders prioritize affordability, accessibility, and responsible use of antibiotics. With regulatory compliance rising to 85%, hospitals will integrate subscription-based pricing within existing frameworks, leading to greater long-term sustainability. ROI from antibiotic subscription models for healthcare providers is projected at 22–28% by 2030, with significant cost savings, reduced waste, and improved treatment outcomes.
Market Analysis
The antibiotic subscription model market in Europe is set to increase from €300 million in 2025 to €1.8 billion by 2030, growing at a CAGR of 45%. This growth is driven by the pressing need for sustainable antibiotic use and the rising burden of antibiotic resistance. By 2030, subscription-based pricing will become the dominant model, reducing over-prescription and encouraging responsible use across hospitals, healthcare systems, and pharmacies. AI-driven stewardship platforms are projected to improve prescription accuracy by 40%, enhancing clinical decision-making and reducing adverse events. Patient adherence is also expected to increase by 20% due to digital subscription models that provide personalized reminders and incentives. The cost per patient for antibiotics is expected to drop 15%, reflecting both pricing innovations and improved supply chain efficiencies. High-cost antibiotic usage is expected to decrease by 25% as pricing becomes more tiered and value-based. Regulatory compliance with GDPR and EU medical frameworks will reach 85% by 2030, ensuring that the model aligns with patient safety and privacy standards. Cross-sector partnerships between biopharma companies, hospitals, and technology providers will help drive model adoption, while pharmaceutical manufacturers will continue to innovate sustainable solutions to meet future demand. ROI for healthcare providers implementing subscription models is estimated at 22–28%, due to the operational efficiency, cost reduction, and improved treatment accessibility these models offer.
Trends & Insights
The antibiotic subscription model market in Europe is growing rapidly, projected to reach €1.8 billion by 2030 at CAGR 45%, driven by the demand for cost-effective, accessible treatments. Key trends include the adoption of tiered subscription pricing that links patient access to cost-efficiency and responsible usage. AI-powered stewardship platforms are central to the model’s success, improving prescription accuracy by 40% and driving a reduction in over-prescription. Antibiotic resistance will decrease by 30% by 2030, thanks to data-driven, patient-specific treatment regimens. Patient adherence is expected to increase by 20% as digital health tools incentivize and monitor therapy completion. Healthcare system adoption is projected at 70%, while regulatory compliance will reach 85%, integrating into EU medical frameworks. The cost per patient for antibiotics will drop by 15%, with AI integration optimizing drug selection and dosage. High-cost antibiotic usage will decrease 25% due to more efficient tier-based access models. Cross-border R&D and data-sharing initiatives will increase by 40% by 2030, leading to more comprehensive, global stewardship. The ROI for healthcare providers implementing these models is estimated at 22–28%, as digital transformation reduces operational inefficiencies, cuts wastage, and improves patient outcomes across the continent.
Segment Analysis
The antibiotic subscription model market in Europe is segmented by pharmaceutical segment (small molecules vs biologics), hospital/clinic type, and technology platform. Small-molecule antibiotics (e.g., cephalosporins, penicillin) will dominate 60% of market share by 2030, as generic versions become more prevalent. Biologic antibiotics will increase 30% in usage, particularly for targeted infection therapies. Public hospitals will drive 70% of adoption, as they look to reduce costs and improve patient access to essential drugs. Private clinics will also adopt the model, albeit at a slower rate, contributing 15% of market share. The remaining 15% will be made up by long-term care facilities and urgent care centers, where antibiotic management is a priority. AI-driven platforms for patient-specific therapy optimization are expected to account for 50% of the market, with an increasing shift towards real-time, data-driven interventions. NLP-based algorithms will streamline prescription workflows, reduce errors, and promote diversity in antibiotic selection. Regulatory compliance will grow to 85% as EU medical frameworks adapt to subscription models. ROI for health systems is projected at 22–28%, driven by improved cost containment, reduced inefficiencies, and better patient adherence. Segment analysis shows that subscription-based models will transform antibiotic pricing, making it more sustainable and accessible while improving clinical outcomes across Europe.
Geography Analysis
The antibiotic subscription model market in Europe is projected to grow from €300 million in 2025 to €1.8 billion by 2030, CAGR 45%. The UK will lead adoption, with public health system models expanding 25% annually through NHS integration and national pricing agreements. Germany, France, and Spain will follow as EU hubs for antibiotic stewardship programs. France’s national plan to reduce antibiotic use by 20% by 2030 positions it as a leader in data-driven subscription models, followed by Germany’s direct-pay subscription pilot for chronic infections. Regulatory standards for antibiotic pricing are projected to reach 85% compliance, with EU-wide pricing models set to align with GDPR, ensuring patient safety and privacy. Patient adoption of subscription models will increase 35% by 2030, as digital apps and monitoring platforms improve therapy adherence and engagement. Healthcare system adoption will reach 70% across public and private institutions, driven by government incentives and payer support for outcome-based reimbursement. Cold-chain logistics and telehealth integration will reduce cost per patient by 15%, while AI algorithms optimize prescribing practices and improve patient outcomes. ROI for implementing antibiotic subscription models will range from 22–28%, driven by reduced operational costs, efficiency improvements, and greater access to essential medicines across Europe.
Competitive Landscape
The competitive landscape for antibiotic subscription models in Europe is highly fragmented, with key players including Antibiotix, MedTechRx, and PharmaSustain leading the charge in AI-powered stewardship platforms. These players provide tiered subscription solutions, integrating real-time eligibility parsing with digital adherence tracking. Pharma companies will drive 50% of market share, partnering with health systems to streamline antibiotic access while improving prescribing accuracy. CROs and AI vendors will capture 40% of market share, providing AI-optimized prescription algorithms, predictive analytics, and data-sharing platforms for trial success and real-world applications. CDMOs will leverage new packaging solutions and storage technologies to meet global demand while reducing cold-chain failures. Competition centers on pricing models, data transparency, and customer service, with digital tools increasingly used for patient engagement and real-time compliance tracking. Regulatory bodies will shape market dynamics, with GDPR compliance and EMA regulations ensuring safe, accountable data practices. By 2030, subscription models will dominate the antibiotic landscape, enabling sustainable pricing, equitable access, and improved health outcomes, with Europe leading the way globally in antibiotic stewardship.
Report Details
Proceed To Buy
Want a More Customized Experience?
- Request a Customized Transcript: Submit your own questions or specify changes. We’ll conduct a new call with the industry expert, covering both the original and your additional questions. You’ll receive an updated report for a small fee over the standard price.
- Request a Direct Call with the Expert: If you prefer a live conversation, we can facilitate a call between you and the expert. After the call, you’ll get the full recording, a verbatim transcript, and continued platform access to query the content and more.


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Request Custom Transcript
Related Transcripts


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071













