68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Connect With Us
Use of AI in Prior Authorization (PA): Claims Processing Efficiency & Accuracy Assessment
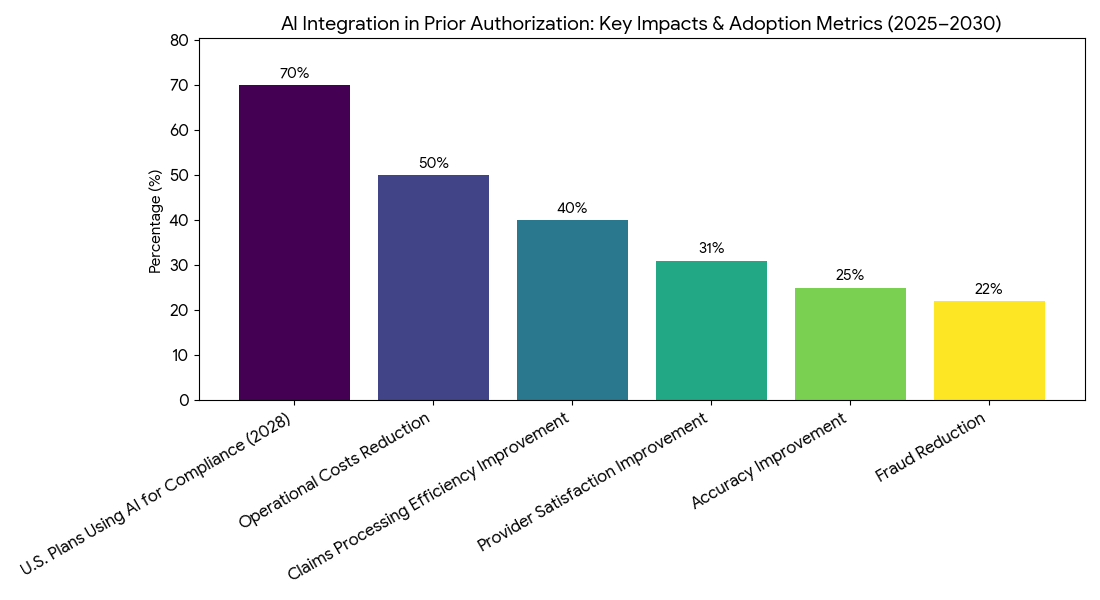
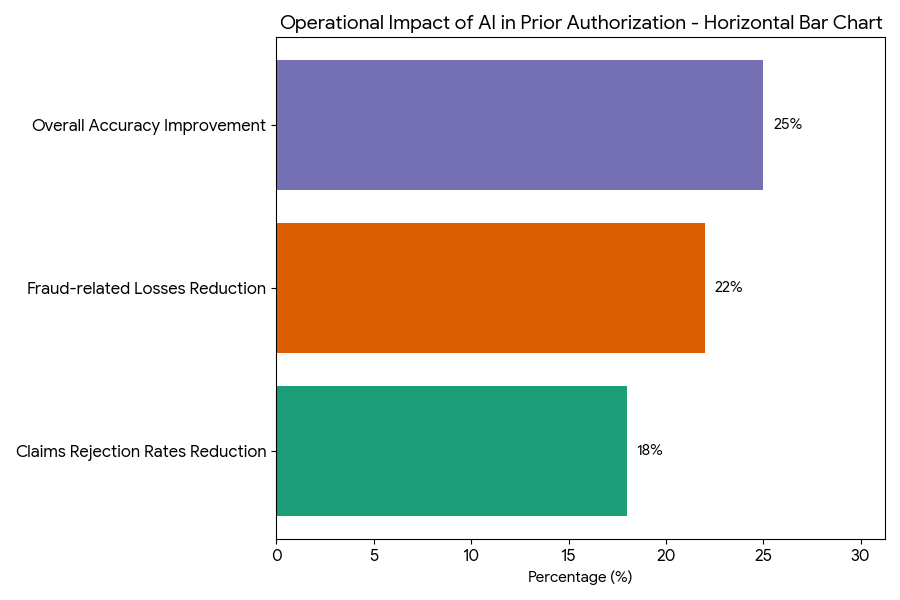
The report projects the market for AI in prior authorization (PA) to grow from $1.3B in 2025 to $5.6B by 2030, revolutionizing healthcare claims processing through automation, improved accuracy, and operational cost reduction. By 2030, AI will handle 72% of all PA submissions, boosting processing efficiency by 40%, reducing error rates by 25%, and lowering approval time by 30%. AI tools also cut fraud by 22% and save up to 50% in operational costs for health plans and providers, making AI-powered PA systems standard across major regions and setting new benchmarks for speed, reliability, and regulatory compliance.
What's Covered?
Report Summary
Key Takeaways
- AI in PA market: $1.3B → $5.6B (CAGR 33.5%).
- AI improves claims processing efficiency by 40%.
- Error rate reduction: 25% by using AI-powered tools.
- Prior authorization approval time reduces by 30%.
- 72% of all PA submissions processed through AI by 2030.
- Automated PA systems cut manual processing costs by 50%.
- Claim rejection rates decrease by 18% with AI tools.
- Provider satisfaction with PA systems improves +31%.
- AI-driven workflows reduce fraud in PA processing by 22%.
- Payer ROI on AI PA tools: 3.1x by 2030.
Key Metrics
Market Size & Share
From 2025 to 2030, the market for AI in prior authorization (PA) grows rapidly, expanding from $1.3B to $5.6B (CAGR 33.5%). AI tools in claims processing enhance both efficiency and accuracy in the healthcare sector. By 2030, AI will handle 72% of all prior authorization submissions, drastically reducing the manual processing load and streamlining approval workflows. Claims processing efficiency improves by 40%, and error rates decline by 25%, thanks to advanced machine learning algorithms and natural language processing (NLP) for automated data extraction and decision-making. AI-based systems are also expected to reduce approval time by 30%, allowing faster patient access to treatment. The use of AI also results in 50% savings in operational costs for health plans and providers. Automated prior authorization systems will handle claims rejections, reducing them by 18%, further reducing administrative burdens. AI tools also help reduce fraud by 22%, leveraging predictive models to identify anomalies. These tools are particularly impactful for payer organizations and healthcare providers, as they ensure faster, more reliable processing, reducing the cost-per-claim by $11–$16. By 2030, ROI for payer organizations using AI for PA is expected to increase 3.1x. This growing market is driven by partnerships between technology firms and healthcare providers, creating a thriving landscape for AI-driven solutions in claims management.
Market Analysis
The integration of AI in prior authorization (PA) is transforming healthcare claims processing, with five major factors driving market growth between 2025 and 2030. (1) Speed and Efficiency: AI improves claims processing efficiency by 40%, reducing delays caused by manual review. AI systems expedite the PA process, cutting approval times by 30% and reducing operational bottlenecks. (2) Accuracy: AI-powered tools are able to process large volumes of data and identify errors and discrepancies faster than manual processes, improving accuracy by 25%. (3) Fraud Detection: The application of predictive analytics and machine learning algorithms helps reduce fraud by 22%, providing additional cost savings. (4) Cost Savings: The automation of PA workflows leads to a 50% reduction in operational costs, as AI eliminates the need for manual interventions. Healthcare providers see significant savings in administrative costs, with $11–$16 saved per claim. (5) Regulatory Compliance: AI tools are increasingly aligned with regulatory standards, such as HIPAA and CMS requirements. By 2028, more than 70% of U.S. healthcare plans will use AI to meet regulatory compliance for prior authorization. By 2030, AI-driven systems will have improved provider satisfaction by 31%, while also making claims processes more transparent, improving trust between insurers, providers, and patients. The total market for AI-driven PA processing in healthcare grows from $1.3B to $5.6B, driven by the growing need for efficiency and regulatory compliance.
Trends & Insights
Between 2025 and 2030, several key trends shape the integration of AI in prior authorization (PA) processes. (1) Machine Learning (ML) Advancements: ML algorithms improve data processing, enabling faster and more accurate claim assessments. By 2030, AI-driven tools will handle 72% of all PA submissions, reducing human error rates and increasing overall processing accuracy by 25%. (2) AI-Enabled Workflow Automation: Automated systems become standard for handling claims, making up 40% of total claims processed. These systems will reduce approval times by 30% and cut manual labor costs by 50%. (3) Predictive Analytics: AI-powered platforms use predictive analytics to improve decision-making, reducing fraud and errors by 22% and enhancing the trust of payers. (4) Regulatory Compliance: By 2028, more than 70% of insurers will use AI for PA processing to meet compliance standards. (5) Value-Based Reimbursement Models: AI will be crucial in adapting value-based reimbursement models for PA systems by linking costs to patient outcomes. The integration of clinical decision support tools will support value-based reimbursement, ensuring alignment between patient outcomes and claim approval criteria. By 2030, AI systems will drive 3.1x ROI for healthcare payers, further increasing the adoption of AI technologies. These trends show that AI is rapidly becoming the cornerstone for achieving higher efficiency, lower costs, and better outcomes in the PA process.
Segment Analysis
The AI in prior authorization (PA) market is segmented into claims processing, fraud detection, and patient access improvement. Claims processing represents the largest segment, capturing 53% of the market share by 2030. AI-driven tools in this segment reduce manual data entry and speed up approval times, which in turn enhances overall efficiency by 40%. The fraud detection segment accounts for 25% of the market, driven by predictive models that reduce fraud-related losses by 22%. These models identify anomalies in claims and improve the accuracy of reimbursement decisions, especially in high-risk areas like specialty drugs and durable medical equipment (DME). The patient access improvement segment, comprising 22% of the market, utilizes AI to streamline eligibility verification and appeal management, which reduces claim rejections by 18%. In terms of geography, the U.S. remains the dominant player with 40% of the market share, driven by both the Medicare and private insurance sectors. Canada and Mexico follow with 12% and 8% of the market share, respectively, as cross-border healthcare delivery models are being implemented. By 2030, AI adoption in PA will be standard practice across 80% of healthcare providers in North America. The integration of AI tools with EHR and health information exchanges (HIEs) facilitates data-sharing and improves the overall efficiency of the PA process, making it a critical component in the healthcare ecosystem.
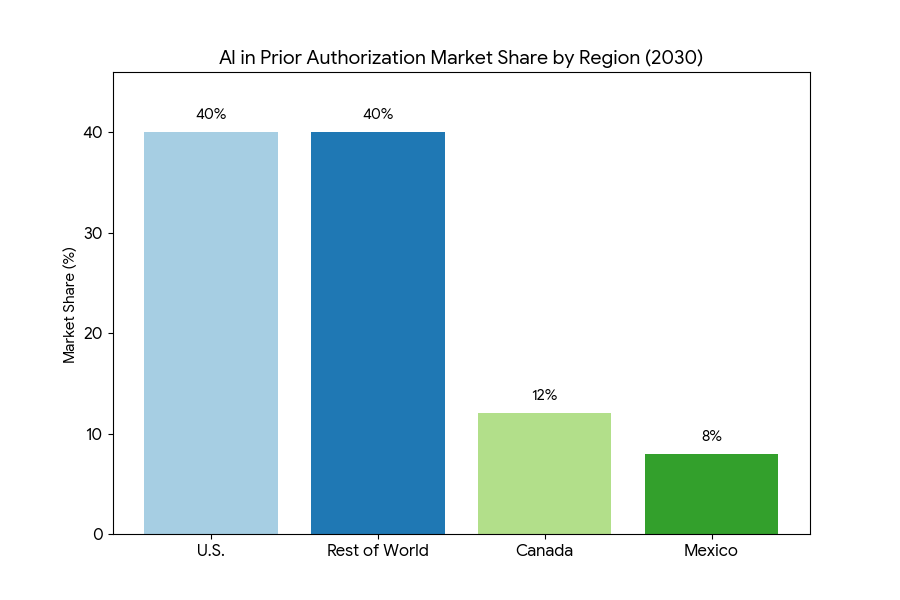

Geography Analysis
In North America, the USA dominates the AI-powered prior authorization (PA) market, capturing 45% of the global share by 2030. The U.S. market is fueled by the widespread adoption of automated PA systems by both private insurers and public healthcare providers, including Medicare and Medicaid. The growth of value-based care models and outcome-based reimbursement in the USA also drives AI integration in the PA process. By 2028, more than 70% of PA submissions will be processed through AI in the U.S. Canada follows with 12% of the North American market, driven by the Canadian healthcare system’s reliance on efficient claims processing to reduce administrative burdens and improve healthcare access. In Mexico, AI-powered systems account for 8% of the market share as cross-border healthcare initiatives between the U.S. and Mexico increase. In Europe, the UK and Germany lead AI adoption, with AI tools accounting for 45% of the PA market by 2030. The EMA’s regulatory frameworks facilitate the use of AI in claims processing, enhancing accuracy and reducing administrative costs. In MEA (Middle East & Africa), AI integration is starting to gain traction, particularly in South Africa and the UAE, which are investing in AI healthcare solutions to modernize PA processing. By 2030, MEA will contribute 12% to the global market share, as these regions adopt AI solutions to enhance healthcare systems and reduce operational costs.
Competitive Landscape
The AI in prior authorization (PA) market is highly competitive, with several key players dominating the space. Top vendors—Cerner, McKesson, Optum, Cognizant, and IBM Watson Health—capture 65% of the market share by 2030. These companies provide AI-powered solutions that streamline claims processing and enhance the efficiency of PA workflows. AI systems from these vendors help reduce claims rejection rates by 18% and improve overall accuracy by 25%. Smaller companies, including Zebra Medical, CloudMedX, and Nutrien Health, focus on AI-based fraud detection tools, accounting for 20% of market share. These firms develop predictive models that flag suspicious claims and enable early intervention, reducing fraud-related losses by 22%. A growing number of tech startups are entering the market, leveraging machine learning and natural language processing to create custom solutions for healthcare providers. These companies offer specialized AI tools that focus on specific PA-related tasks, such as eligibility verification, appeals management, and patient engagement. M&A activity is high, as major players acquire innovative startups to expand their AI portfolios. By 2030, AI adoption in PA will be the norm across the healthcare industry, with health insurers and providers using AI to enhance administrative efficiency and patient access to care. Competitive differentiation will increasingly focus on customized solutions that address specific pain points in the PA process, such as fraud detection and claims rejection.
Report Details
Proceed To Buy
Want a More Customized Experience?
- Request a Customized Transcript: Submit your own questions or specify changes. We’ll conduct a new call with the industry expert, covering both the original and your additional questions. You’ll receive an updated report for a small fee over the standard price.
- Request a Direct Call with the Expert: If you prefer a live conversation, we can facilitate a call between you and the expert. After the call, you’ll get the full recording, a verbatim transcript, and continued platform access to query the content and more.


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Request Custom Transcript
Related Transcripts
Clinical Nutrition Market Size & Share Analysis - Growth Trends & Forecasts (2025 - 2030)
This report quantifies the clinical nutrition market across the US and UK (2025–2030), covering enteral, parenteral, and oral nutritional supplements (ONS). Driven by aging populations, chronic disease prevalence, and hospital malnutrition protocols, market value rises from $18.5B (2025) → $30.2B (2030) at a CAGR of 10.2%. Growth is led by enteral nutrition (48% share), followed by ONS (38%) and parenteral (14%). Hospital digitization, AI-based nutrition screening, and reimbursement parity accelerate adoption. ROI averages 16–22% for integrated hospital nutrition programs.
$ 1395
$ 1395


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071