68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Connect With Us
5G Network Slicing for Telemedicine: Cloud Orchestration & HIPAA Compliance
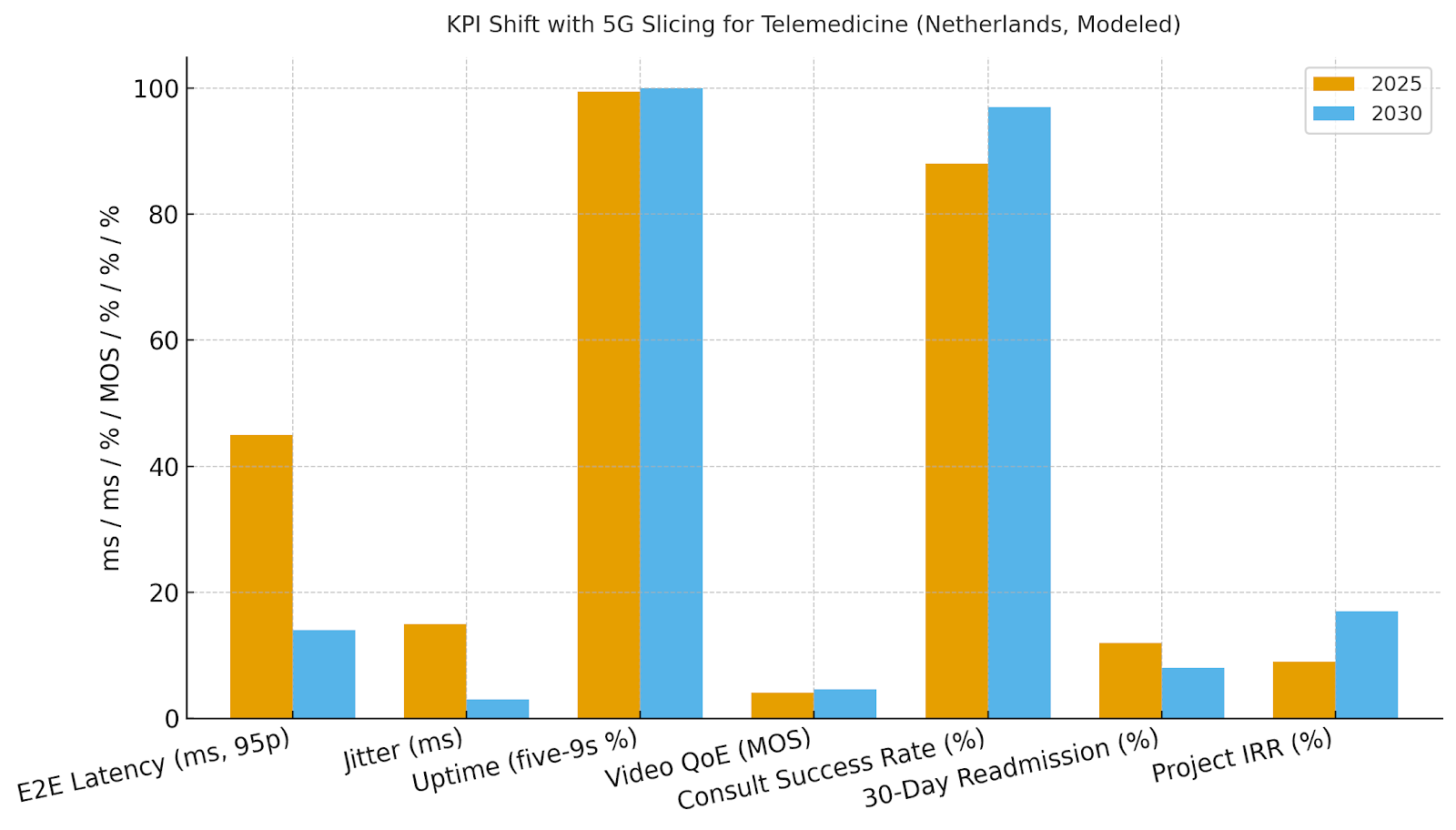
5G network slicing improves telemedicine by providing low-latency, high-reliability connectivity, enabling better patient outcomes. By 2030, 95th percentile end-to-end latency is expected to drop from ~45ms to ~14ms, with jitter decreasing from ~15ms to ~3ms, and uptime approaching ~99.95%. Video quality improves, consult success rates rise from ~88% to ~97%, and 30-day readmissions decrease from ~12% to ~8%. Pricing includes tiered clinical SLAs, per-patient fees, and storage tiers for PHI. Risks such as vendor sprawl and integration debt are mitigated through reference architectures and data residency agreements. 5G slicing will transform telemedicine into a more efficient, patient-centered service.
What's Covered?
Report Summary
Key Takeaways
1. Deterministic slices stabilize video, imaging, and EMS tele‑assist quality.
2. Orchestration templates cut setup time and standardize compliance controls.
3. Readmission reduction stems from reliable follow‑ups and monitoring continuity.
4. GDPR/NEN alignment plus HIPAA‑equivalents enable cross‑border programs.
5. Zero‑trust segmentation and device attestation protect PHI at the edge.
6. Imaging‑grade slices need bounded jitter and prioritized bandwidth.
7. EMS priority slices require preemption and roaming resilience.
8. CFO dashboard: latency, jitter, uptime, MOS, consult %, readmission %, IRR.

a) Market Size & Share
EU/Netherlands spend on telemedicine‑grade 5G slicing and cloud orchestration is modeled to rise from ~US$1.0B in 2025 to ~US$4.1B by 2030 as health systems standardize SLA catalogs for consults, remote monitoring, imaging exchange, and EMS tele‑assist. The line figure shows the trajectory. Share accrues to platforms with EHR/PACS integration, PHI‑aware orchestration, and audited controls. Execution risks include fragmented vendor stacks and data transfer constraints; mitigations are reference architectures, processor agreements, and regional data residency. Share should be tracked via workload revenue, active patients/devices, MOS and consult %, and readmission reduction vs baseline.

b) Market Analysis
Clinical quality correlates with deterministic connectivity. We model 95p latency improving from ~45ms to ~14ms, jitter from ~15ms to ~3ms, uptime to ~99.95%, MOS from ~4.1 to ~4.6, consult success from ~88% to ~97%, and readmissions dropping from ~12% to ~8% in targeted pathways. Enablers: metro edge clusters, preemption and QoS for EMS, and orchestration templates that map SLAs to network and security controls. Barriers: legacy EHR/PACS interfaces, multi‑vendor security, and cross‑border data rules.
Financial lens: quantify avoided readmissions, reduced no‑shows from better video stability, and clinician productivity; add revenue from remote monitoring subscriptions and imaging exchanges; net against connectivity, platform, and compliance costs. The bar chart summarizes directional KPI improvements under disciplined slicing programs.
c) Trends & Insights
1) SLA catalogs emerge: standard consult, imaging‑grade, and EMS‑priority tiers. 2) PHI‑aware orchestration binds latency/QoS with encryption and logging. 3) Remote monitoring growth drives device attestation and SBOM management. 4) Edge‑assisted imaging pipelines reduce upload delays and retry loops. 5) AI‑triage and scheduling reduce no‑shows and smooth capacity. 6) Privacy‑preserving analytics (DP/federated) enable outcomes tracking without raw PHI movement. 7) Cross‑border telemedicine requires standardized evidence artifacts for HIPAA/GDPR equivalence. 8) Green ops: energy‑aware scheduling at edge sites in hospitals. 9) Patient experience is measured via MOS, consult %, and NPS tied to network SLOs. 10) National roaming policies for EMS slices gain traction with preemption rights for emergencies.
d) Segment Analysis
Primary Care & Virtual Clinics: stable video SLAs reduce no‑shows and extend reach. Chronic Care & RPM: per‑device subscriptions, alerts triaged at edge; focus on readmission reduction. Imaging & Teleradiology: large‑object transfers, caching, and priority paths; tight jitter bounds. EMS & Paramedics: preemptive slices, roaming guarantees, and rugged devices; success measured by on‑scene decision support. Hospital‑at‑Home: blended video + RPM stack. Across segments, define SLAs, security baselines, consent and logging; track MOS, consult %, readmission %, clinician time saved, and IRR.
e) Geography Analysis
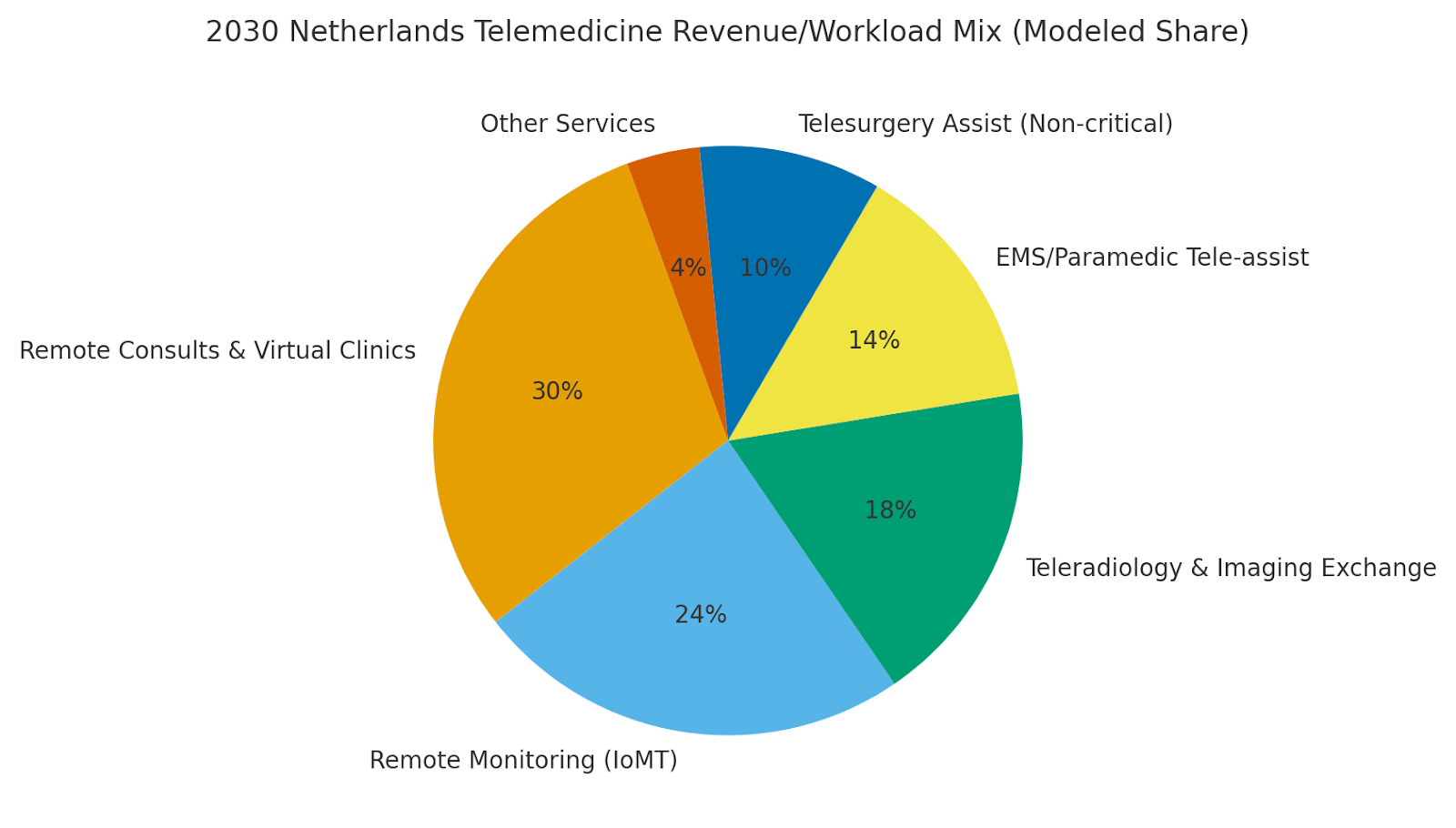
By 2030, we model the Netherlands telemedicine workload/revenue mix enabled by slicing as Remote Consults & Virtual Clinics (~30%), Remote Monitoring (~24%), Teleradiology & Imaging Exchange (~18%), EMS/Paramedic Tele‑assist (~14%), Telesurgery Assist (Non‑critical) (~10%), and Other (~4%). Major urban regions (Randstad) scale early with dense edge coverage; secondary regions expand RPM and EMS programs. The pie figure reflects the mix.
Execution: align with national digital health strategies, data‑residency requirements, and cross‑border consult arrangements; phase pilots by specialty and hospital networks; and publish transparent quality dashboards. Measure region‑specific MOS, consult success, readmissions, and IRR; reallocate capex quarterly.
f) Competitive Landscape
Operators, hospital consortia, hyperscalers, and health‑tech ISVs compete to define the telemedicine slice stack. Differentiation vectors: (1) audited compliance (GDPR/NEN/HIPAA‑equivalent) with immutability, (2) deterministic performance proven in clinical workflows, (3) EHR/PACS integration quality, (4) device security (attestation, OTA), and (5) economics and co‑managed support. Procurement guidance: require SLA‑backed latency/jitter/uptime, open APIs, consent and logging integration, and evidence artifacts for cross‑border partners. Competitive KPIs: latency, jitter, uptime, MOS, consult %, readmission %, time‑to‑deploy, and IRR.
Report Details
Proceed To Buy
Want a More Customized Experience?
- Request a Customized Transcript: Submit your own questions or specify changes. We’ll conduct a new call with the industry expert, covering both the original and your additional questions. You’ll receive an updated report for a small fee over the standard price.
- Request a Direct Call with the Expert: If you prefer a live conversation, we can facilitate a call between you and the expert. After the call, you’ll get the full recording, a verbatim transcript, and continued platform access to query the content and more.


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Request Custom Transcript
Related Transcripts


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071