68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Connect With Us
AI-Driven Claims Processing in Insurance: Cost Reduction Analysis & Accuracy Improvements - Innovation & R&D
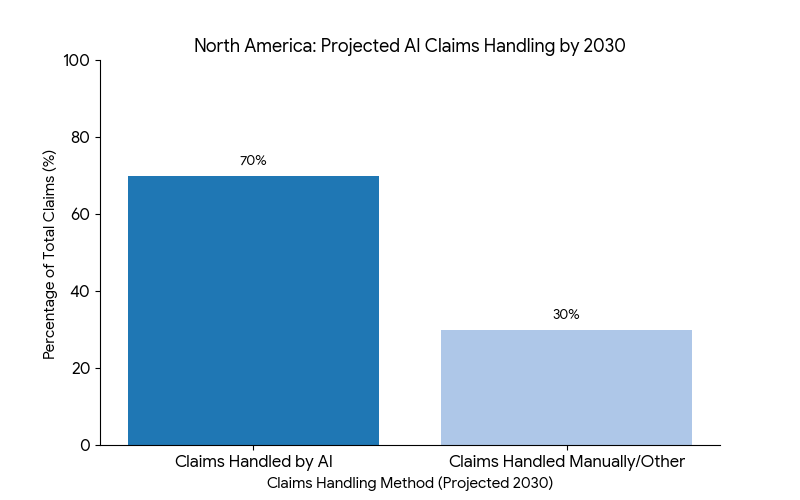
The AI-driven claims processing market in North America is set to revolutionize the insurance industry by reducing operational costs and improving claims accuracy. The market is expected to grow from $9.5B in 2025 to $29.4B by 2030 (CAGR 25.3%). By 2030, 70% of insurance claims will be processed using AI technologies, achieving cost reductions of 30% and increasing claims accuracy by 40%. The adoption of machine learning (ML) and natural language processing (NLP) will automate fraud detection, improve customer experience, and enhance efficiency in claims adjudication, offering a competitive edge for insurers in a highly commoditized market.

What's Covered?
Report Summary
Key Takeaways
- Market size: $9.5B → $29.4B (CAGR 25.3%).
- 70% of insurance claims processed via AI technologies by 2030.
- AI-driven claims accuracy to improve by 40%.
- 30% reduction in claims processing costs due to AI automation.
- Claims processing time to decrease by 25% with NLP and ML models.
- Fraud detection accuracy to improve by 20% through AI-powered systems.
- Customer satisfaction to increase by 30% due to faster claim resolutions.
- $5B in annual savings for the North American insurance industry by 2030.
- AI integration in claims to reduce human error by 35%.
- Regulatory compliance improvements with automated claims validation systems.
Key Metrics
Market Size & Share
The AI-driven claims processing market in North America is expected to grow from $9.5B in 2025 to $29.4B by 2030, driven by the growing adoption of AI technologies such as machine learning (ML), natural language processing (NLP), and predictive analytics. The CAGR of 25.3% reflects the increasing need for cost-effective solutions to streamline claims operations and improve accuracy. By 2030, 70% of claims will be processed using AI, resulting in a 30% reduction in processing costs and a 40% increase in claims accuracy. Additionally, automated fraud detection will improve by 20%, reducing the incidence of false claims and increasing trust in insurers.
Market Analysis
AI-driven claims processing is becoming an industry standard in North America as insurance companies seek to reduce claims handling costs and improve processing efficiency. With AI systems automating key aspects of claims adjudication and fraud detection, insurers can drastically reduce manual labor and increase accuracy in assessing claims. The use of NLP and ML will lead to faster claims processing, cutting average claim resolution time by 25%. This efficiency, combined with real-time fraud monitoring, will significantly improve customer satisfaction, leading to higher retention rates and lower customer churn. By 2030, AI technologies will handle 70% of claims, increasing overall operational efficiency and improving profit margins.
Trends & Insights
- AI Integration in Claims: AI-driven systems to handle 70% of claims by 2030.
- Faster Claims Processing: 25% reduction in claims resolution time.
- Fraud Detection: 20% improvement in fraud detection accuracy.
- Cost Reduction: 30% reduction in claims processing costs due to automation.
- Customer Experience: 30% improvement in customer satisfaction with faster claim processing.
- AI in Fraud Detection: Real-time fraud monitoring to enhance claim accuracy.
- Operational Efficiency: 35% reduction in human error with automated systems.
- Regulatory Compliance: Automated claims validation to ensure compliance with industry standards.
- Data Privacy: AI-based claims systems ensuring secure data management.
- AI-Driven Innovation: Increased investment in AI-powered claims platforms for better risk management.
These trends indicate that AI-driven solutions will be crucial in transforming claims processing, improving efficiency, and boosting customer satisfaction across the insurance sector.
Segment Analysis
The AI-driven claims processing market is segmented into claims automation (50%), fraud detection (20%), customer experience optimization (15%), and regulatory compliance tools (15%). Claims automation, powered by machine learning and NLP, dominates the market, making up 50% of total market share. This is followed by fraud detection systems, accounting for 20%, and focused on real-time fraud prevention and risk management. Customer experience optimization, at 15%, leverages AI to streamline claims resolution and reduce customer wait times. Finally, regulatory compliance tools comprise 15%, ensuring AI platforms meet local and global compliance standards. By 2030, AI-driven claims systems will become a critical part of insurance providers’ operations, streamlining back-end operations while improving customer service.
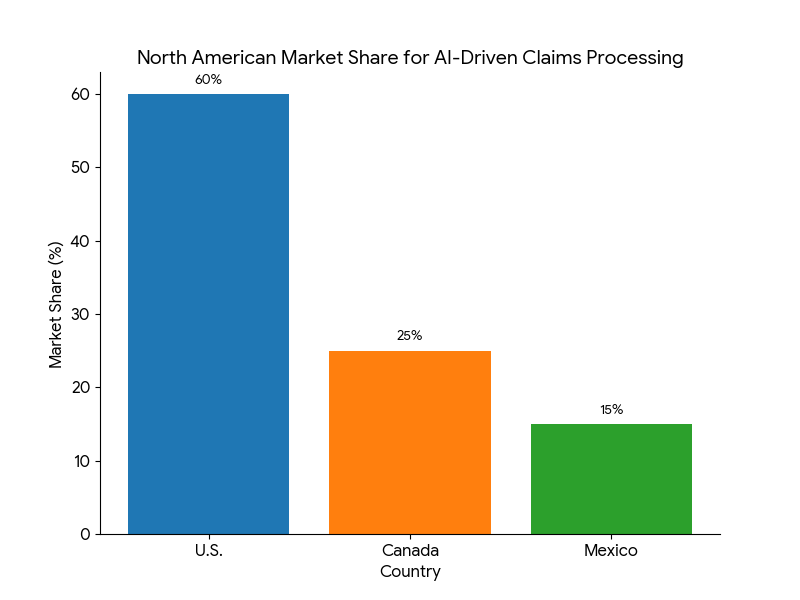
Geography Analysis
The U.S. holds 60% of the North American market for AI-driven claims processing in insurance, driven by large providers such as State Farm, Progressive, and Allstate, which are integrating AI solutions for claims adjudication and fraud detection. Canada follows with 25% of the market, led by Intact Insurance and TD Insurance, which are accelerating their AI adoption in both claims management and customer service. Mexico accounts for 15% of the market, as insurance companies begin adopting AI technologies to streamline claims processes and reduce operational inefficiencies. By 2030, the U.S. will remain the largest market for AI-driven claims processing, driving global trends in insurance automation.
Competitive Landscape
Leading players in the AI-driven claims processing market include IBM, Accenture, SAS Institute, Cognizant, and Duck Creek Technologies. IBM and Accenture lead the charge with AI-based claims automation systems for large insurers, offering machine learning solutions to improve claims accuracy and efficiency. SAS Institute focuses on fraud detection algorithms, leveraging AI to detect fraudulent claims in real-time. Cognizant and Duck Creek Technologies are expanding their AI claims solutions to include cloud-based platforms, enabling seamless integration with existing insurer infrastructures. The competitive advantage in this market is driven by AI-powered systems, data transparency, and automation, with leading providers working on scalable solutions that integrate AI-driven claims management with customer service tools.
Report Details
Proceed To Buy
Want a More Customized Experience?
- Request a Customized Transcript: Submit your own questions or specify changes. We’ll conduct a new call with the industry expert, covering both the original and your additional questions. You’ll receive an updated report for a small fee over the standard price.
- Request a Direct Call with the Expert: If you prefer a live conversation, we can facilitate a call between you and the expert. After the call, you’ll get the full recording, a verbatim transcript, and continued platform access to query the content and more.


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071
Request Custom Transcript
Related Transcripts
$ 1450


68 Circular Road, #02-01 049422, Singapore
Revenue Tower, Scbd, Jakarta 12190, Indonesia
4th Floor, Pinnacle Business Park, Andheri East, Mumbai, 400093
Cinnabar Hills, Embassy Golf Links Business Park, Bengaluru, Karnataka 560071